
Florida’s current spotlight centers around a measles outbreak that has especially impacted children. Dr. Joseph Ladapo’s unorthodox approach to managing this crisis adds a layer of complexity. Let’s embark on a comprehensive journey to decipher the intricacies of the outbreak, the factors fueling it, the nuances of measles vaccination, and the perils tied to letting unvaccinated children roam freely in schools.
The Current Outbreak in Florida
Florida finds itself in the midst of a measles outbreak, predominantly affecting children. Measles, notorious for its contagious nature, poses a substantial threat, especially to the unvaccinated population. Dr. Ladapo’s departure from CDC guidance challenges the recommended 21-day isolation period for unvaccinated children post-exposure, adding a unique twist to the unfolding narrative.
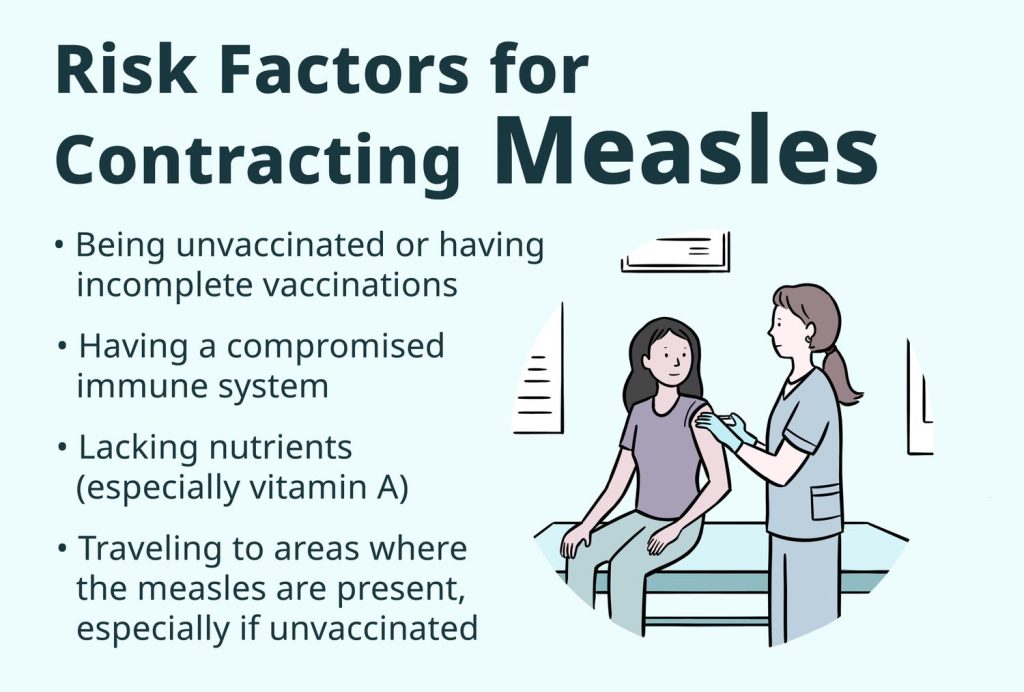
Factors Influencing Measles Outbreaks
To grasp the roots of this outbreak, a closer look at measles vaccination rates becomes imperative. The CDC’s data reveals that only about 93% of kindergarten students received the measles vaccine in the 2021-2022 school year, falling below the targeted 95%. This vaccination gap serves as fertile ground for outbreaks, not only in Florida but also in regions densely populated with unimmunized children.

The domino effect of declining vaccination rates magnifies the risk. It’s not merely about individual vulnerability; it’s about collective immunity necessary to shield entire communities. The current outbreak in Florida is a stark reminder of the repercussions when herd immunity wavers.
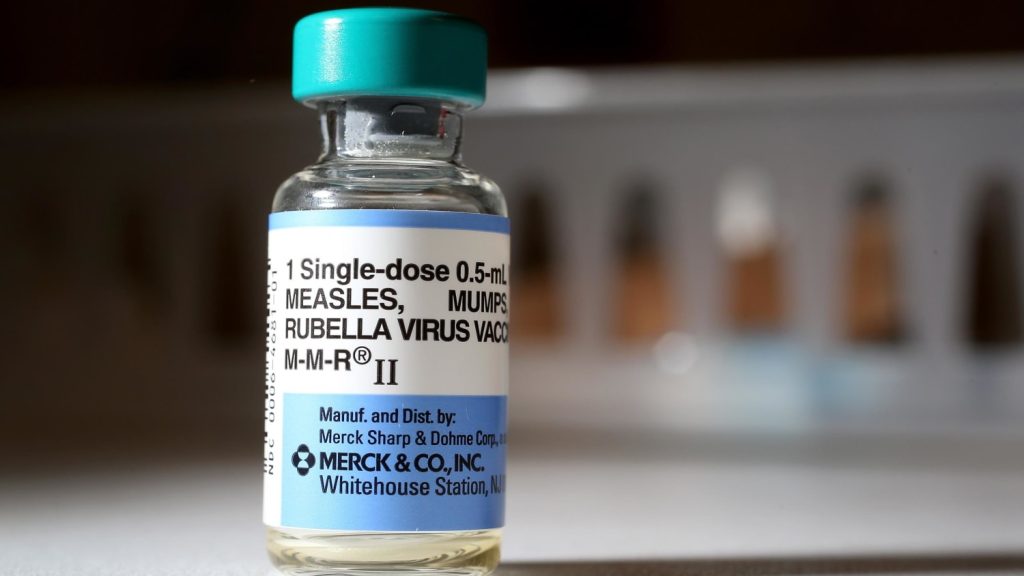
Effectiveness of the Measles Vaccine
While vaccines are pivotal in disease prevention, acknowledging their limitations is equally crucial. The measles vaccine, although highly effective, does not provide an absolute guarantee of protection. This becomes paramount when contemplating the achievement of herd immunity. Failure to attain the desired vaccination coverage leaves more individuals susceptible to the virus, creating pockets of vulnerability that can spark outbreaks.

The Florida scenario accentuates the need to communicate not only the personal benefits of vaccination but also the communal responsibility it entails. The effectiveness of the vaccine hinges on widespread adoption, making it imperative to bridge the gap in vaccination rates to ensure robust herd immunity.
Risks Associated with School Attendance
Allowing unvaccinated children to attend school during an outbreak poses significant risks. The dynamic and interactive nature of school environments provides an ideal setting for a highly contagious virus like measles to spread rapidly. Experts stress that continuing to send unvaccinated kids to school heightens the risk, not only for those children but for the broader community.
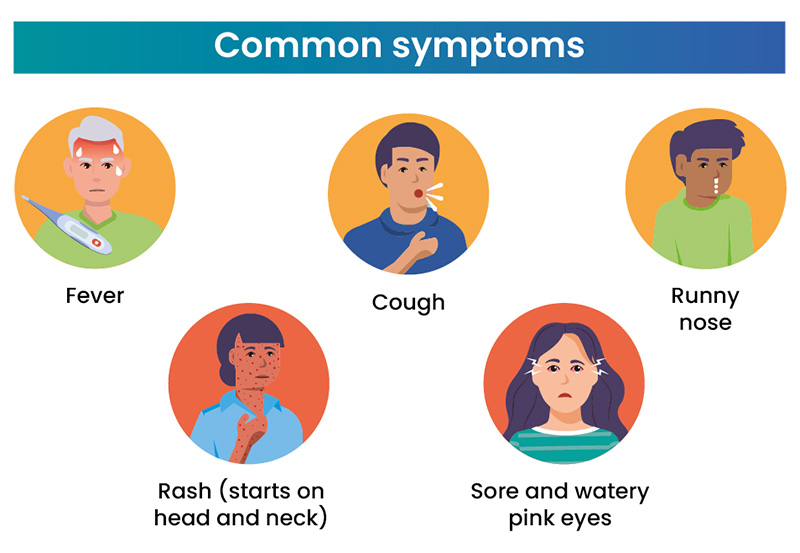
The interconnectedness of communities in schools amplifies the potential for measles to gain a foothold. It’s not merely an individual decision but one that impacts collective well-being. The choice to keep unvaccinated children at home during an outbreak aligns with the CDC’s recommendations, emphasizing the importance of community-wide efforts in curbing the spread of infectious diseases.

The measles outbreak in Florida serves as a microcosm of a broader public health challenge. It’s not just about managing the current cases but addressing the root causes of declining vaccination rates. Dr. Ladapo’s deviation from CDC guidance adds a layer of complexity to the situation, highlighting the need for unified and science-based approaches.

As we navigate the complexities of this outbreak, it’s crucial to recognize the interconnectedness of our communities. Measles is not a concern confined to Florida alone; it’s a collective challenge that requires collective solutions. Bridging the gap in vaccination rates, dispelling myths surrounding vaccines, and reinforcing the importance of community health are pivotal steps toward creating a safer and more resilient society.





GIPHY App Key not set. Please check settings